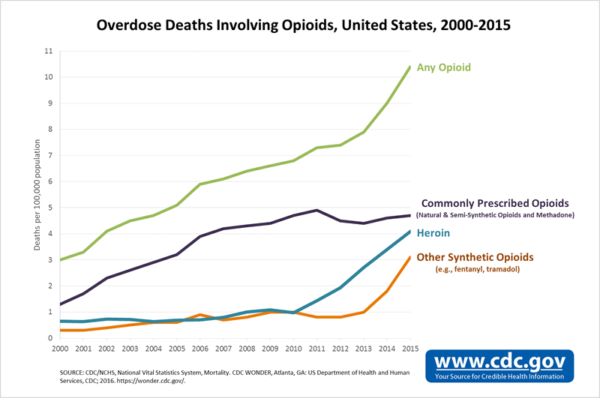
In October 2017, President Trump declared the opioid epidemic a National Public Health Emergency. Three months later, it was confirmed that drug overdose deaths had increased significantly in 2016 to more than 63,600, with more than 42,200 attributed to opioids.[1] This raises a plethora of questions— How did we get here? What exactly is a National Public Health Emergency? Is it enough to solve the epidemic? What does it mean for the insurance industry?
Recent trends contributing to the growing opioid epidemic
The opioid epidemic refers to the rapid increase in the usage of and addiction to prescription and non-prescription opioids. While every day seems to bring another news article highlighting a new issue relating to opioids, there are three major reasons why the epidemic has become so widespread:
(1) Many believe prescription opioids are being prescribed too freely. According to the 2017 Annual Surveillance Report of Drug-Related Risks & Outcomes by the CDC National Center for Injury Prevention & Control, doctors wrote 66.5 opioid prescriptions per 100 persons in 2016.[2]
(2) The number of overdose deaths in the U.S. from fentanyl has increased in the past few years. Some people are prescribed pharmaceutical fentanyl, but most fentanyl-related harm involves illegally made fentanyl sold on the illegal drug market. Fentanyl is extremely potent and many times it is mixed with other drugs without the user’s knowledge, which is extremely dangerous.
(3) While heroin used to be found only in urban communities among the poor, heroin is now also impacting rural areas and wealthy suburban communities.
Recent News the Insurance Industry Should Know
There is no question the opioid epidemic is costly for insurance companies. As such, many companies have implemented new practices and procedures. Furthermore, insurance companies may be impacted by both governmental decisions and legal actions in connection with the opioid epidemic. Here are some highlights of recent news involving or impacting the insurance industry:
- Although the federal government was initially poised to classify the opioid epidemic as a National Emergency, on October 26, 2017, President Trump declared it a National Public Health Emergency.
- If Trump had declared the opioid epidemic a National Emergency, the federal government would have had access to funds from FEMA. By declaring it merely a National Public Health Emergency, no additional federal funding will be automatically available; rather, federal agencies will be directed to use grant money already in their budgets to address the opioid epidemic.[3]
- Many believe the federal government’s response is not enough, and that other industries, such as the insurance industry, will need to step up and find solutions.
- In November 2017, sixteen major healthcare providers agreed to adopt “National Principles of Care” for the treatment of addition.
- This group of providers includes six of the largest payers in the U.S. and covers over 248 million patients.[4]
- The eight principles include universal screening for substance abuse disorder, personalized diagnosis, access to qualified health professionals, and access to non-medical recovery support services.
- The workers’ compensation industry has made some progress combating the epidemic.
- Many states have attempted to curb opioid use by creating “drug formularies.” Other states, such as California, will begin implementing “drug formularies” as of January 1, 2018.[5]
- Express Scripts Holding Co. found that it lowered prescription drug spending on workers compensation payers by 7.6% in 2016, which accounted for a second-year decline in opioid prescribing.[6]
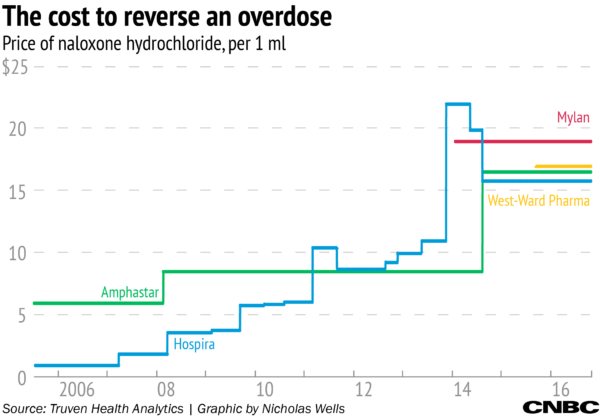
- Naloxone can reverse an overdose. But as overdose deaths spike, pharmaceutical companies have raised naloxone’s average wholesale price.
- Aetna announced that beginning January 1, 2018, it will waive the co-pay of Narcan, the brand name version of the naloxone nasal [7]
- The waived co-pay only applies to Aetna’s fully-insured commercial members, who get their health coverage through an employer.
- Some studies have suggested that one potential solution to the epidemic is to prescribe medical marijuana to injured people rather than prescription opioids. There is a split of authority, however, as to whether medical marijuana expenses are reimbursable under workers’ compensation laws.
- At least five states—Connecticut, Maine, Minnesota, New Jersey and New Mexico—have found medical marijuana treatment is reimbursable under their workers compensation laws. But a few states, such as Florida and North Dakota, have passed laws excluding medical marijuana treatment from workers’ compensation reimbursement.
- As insurance companies and government entities initiate new treatment opportunities to assist individuals addicted to opioids, insurance companies should be aware of increasing cases of insurance fraud.
- As an example, brokers have fraudulently procured insurance policies for addicts and subsequently sent the addict to an out-of-state treatment center. These treatment centers then billed insurance companies large sums of money, while in reality the treatment centers were only providing poor quality treatment to the addict.
- Lawyers and state and local governments have initiated lawsuits against Big Pharma. The general allegations in these suits is that opioid drug-makers engaged in fraudulent marketing; this marketing then led to addiction among patients and also resulted in addiction to heroin as patients sought illegal drugs when painkillers were no longer available. Now, taxpayers are funding public health and law enforcement costs.
- In 2017, some pharmaceutical companies began settling these lawsuits. For example, in January 2017, Cardinal Health (largest supplier of drugs in West Virginia) and AmerisourceBergen (3rd largest supplier of drugs in West Virginia) agreed to pay $36 million to settle lawsuits alleging that these companies benefitted from West Virginia’s problem with prescription drug abuse.[8]
- New lawsuits are still being filed against these companies. For example, in December 2017, towns and counties in Illinois, Nevada, Iowa and Massachusetts filed lawsuits against manufacturers and distributors.
- Recently, shareholders have filed a series of lawsuits against opioid manufacturers and distributors and their directors and officers. These suits generally allege that the companies were engaging in questionable practices that would likely subject them to legal and regulatory scrutiny and that they made materially false representations.[9]
- Insurance companies that provide coverage to these pharmaceutical companies may not owe their insureds a defense, although it will likely depend on the applicable policy wording. At the end of 2017, in Travelers Prop. Cas. Co. of America v. Actavis, Inc., 16 Cal.App.5th 1026 (Cal. Ct. App. Nov. 6, 2017), a California appellate court affirmed that Travelers had no duty to defend under comprehensive general liability policies issued to Actavis LLC and other pharmaceutical companies. Local California and Chicago governments had sued these defendants for fraud and misrepresentation arising out of a “highly deceptive marketing campaign.” The court held that Travelers’ denial of coverage was proper because the alleged injuries were caused by “deliberate and intentional conduct” rather than by an “accident.” Additionally, the suit’s claims fell within the policies’ products exclusion and were thus excluded from coverage.
Where Do We Go From Here?
As we head into 2018, everyone is in agreement that the opioid epidemic is a real issue that is costing the government, insurance companies, and taxpayers a lot of money. While there have been some positive signs the country is heading in the right direction—for example, there was less prescription spending in the workers’ compensation industry—it is difficult to determine if enough is being done, and if not, where the best place to focus truly lies. Should we focus on prescribing practices? On shutting down the illegal drug market? Or on treatments for those already addicted? Many questions still remain, but as federal, state, and local governments are currently spending resources on a wide variety of potential solutions, we have an opportunity to monitor the situation throughout the year and hopefully gain better insights into how to put an end to the epidemic.
Disclaimer: This article is provided solely as a reference tool to be used for informational purposes only. The information in this article shall not be construed or interpreted as providing legal or any other advice. Use of this article for any purpose other than as set forth herein is strictly prohibited.
[1] Centers for Disease Control and Prevention, Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. MMWR 2016: 65(50-51);1445–1452.
[2] Centers for Disease Control and Prevention, Annual Surveillance Report of Drug-Related Risks & Outcomes, United States, 2017, https://www.cdc.gov/drugoverdose/pdf/pubs/2017-cdc-drug-surveillance-report.pdf
[3] Dan Merica, Trump Declares Opioid Epidemic a National Public Health Emergency, CNN Politics (October 26, 2017) http://www.cnn.com/2017/10/26/politics/donald-trump-opioid-epidemic/index.html
[4] Bruce Y. Lee, 16 Insurance Companies Make Commitment to Address Opioid Crisis, Forbes (Nov. 9, 2017) https://www.forbes.com/sites/brucelee/2017/11/09/16-insurance-companies-make-commitment-to-address-opioid-crisis/#5da0fb8279de
[5] Louisa Esola, Moving Forward with Comp Drug Formulary Starting Jan. 1, Business Insurance (Dec. 8, 2017) http://www. businessinsurance.com/article/20171208/NEWS08/912317818/California-moving-forward-with-comp-drug-formulary-starting-Jan-1
[6] Press Release, U.S. Worker’s Compensation Prescription Drug Spending Decreased 7.6% in 2016 Through Cost-Savings Solutions, Improved Care for Injured Workers, Business Insider (April 4, 2017) http://markets.businessinsider.com/news/ stocks/U-S-Workers-Compensation-Prescription-Drug-Spending-Decreased-7-6-in-2016-Through-Cost-Savings-Solutions-Improved-Care-for-Injured-Workers-1001893821
[7] Kimberly Leonard, Health Insurer Aetna Announced Tues that it Will Provide Narcan to Some of its Customers at No Costs,, Ohio Society of Addiction Medicine (Dec. 14, 2017) https://ohsam.org/2017/12/14/aetna-announced-that-it-will-provide-narcan-at-no-cost/
[8] Eric Eyre, 2 drug distributors to pay $36M to settle WV painkiller lawsuits, Charleston-Gazette Mail (Jan.1, 2017) https://www.wvgazettemail.com/news/health/drug-distributors-to-pay-m-to-settle-wv-painkiller-lawsuits/article_b43534bd-b020-5f56-b9f3-f74270a54c07.html
[9] Kevin LaCroix, Securities Suits Hit Opioid Drug Companies, The D&O Diary (Sept. 5, 2017) https://www.dandodiary.com /2017/09/articles/securities-litigation/securities-suits-hit-opioid-drug-companies/